The Urgent Need For Better Mental Health Care

Table of Contents
The Accessibility Crisis in Mental Healthcare
Access to mental healthcare remains a significant hurdle for many, creating a profound accessibility crisis. This lack of access stems from a complex interplay of geographic, financial, and systemic barriers.
Geographic Barriers
Many individuals, particularly those in rural areas and underserved communities, face significant challenges accessing mental health professionals. The sheer distance to services presents a considerable obstacle.
- Long travel distances: Rural populations often live far from mental health clinics and hospitals, requiring lengthy and potentially costly commutes.
- Limited transportation options: Lack of reliable public transportation or personal vehicles further restricts access for those without private means of travel.
- Lack of specialized services: Rural areas frequently lack specialized mental health services for conditions like severe mental illness or eating disorders.
For instance, a recent study revealed that individuals in rural counties have 60% fewer mental health professionals compared to their urban counterparts, highlighting the stark disparity in access. This geographical limitation directly impacts timely intervention and treatment adherence, worsening the severity of mental health conditions.
Financial Barriers
The high cost of mental healthcare is a major deterrent, preventing many from seeking or continuing necessary treatment.
- High insurance premiums: Many insurance plans have high premiums and deductibles, making mental healthcare prohibitively expensive.
- Limited insurance coverage for mental health: Even with insurance, coverage for mental health services is often limited, leading to significant out-of-pocket costs.
- Expensive out-of-pocket costs: The cost of therapy sessions, medication, and hospitalization can quickly accumulate, creating a substantial financial burden for individuals and families.
The financial burden of mental healthcare frequently leads to delayed treatment, compromised treatment adherence, and ultimately, poorer health outcomes. This financial barrier disproportionately affects lower-income individuals and families, exacerbating existing health disparities.
Systemic Barriers
Beyond geographic and financial barriers, systemic issues within the healthcare system further complicate access to mental healthcare.
- Bureaucracy in accessing services: Navigating complex referral processes and insurance authorizations can be a time-consuming and frustrating experience.
- Lack of coordination between different healthcare providers: Poor communication and coordination between primary care physicians, specialists, and mental health providers can lead to fragmented care and delays in treatment.
- Long wait times for appointments: Many individuals face extensive wait times to see mental health professionals, delaying crucial interventions.
These systemic inefficiencies create significant obstacles, hindering timely access to vital mental health services. Streamlining referral processes, improving inter-provider communication, and reducing wait times are crucial steps towards improving accessibility.
The Stigma Surrounding Mental Illness
The pervasive stigma surrounding mental illness is a major barrier to help-seeking. Negative attitudes and misconceptions contribute to delayed or avoided treatment, perpetuating the cycle of suffering.
Societal Attitudes and Misconceptions
Deep-rooted societal attitudes and misconceptions fuel the stigma surrounding mental illness.
- Negative stereotypes: Mental illness is often portrayed as a character flaw or a sign of weakness, leading to prejudice and discrimination.
- Fear of judgment: The fear of being judged or ostracized by family, friends, or colleagues prevents many from seeking help.
- Discrimination: Individuals with mental health conditions face discrimination in employment, housing, and social interactions.
These negative perceptions create a climate of silence and secrecy, preventing open conversations about mental health and hindering access to support.
The Role of Media and Public Discourse
Media portrayals and public conversations significantly influence perceptions of mental illness.
- Sensationalized reporting: Media often focuses on sensationalized aspects of mental illness, perpetuating harmful stereotypes and fostering fear.
- Lack of accurate information: Inaccurate or incomplete information about mental health conditions contributes to misunderstandings and misinformation.
- Harmful stereotypes: Media often portrays individuals with mental illness in a negative or stereotypical manner, reinforcing harmful biases.
Responsible and accurate reporting is essential to combat stigma and promote understanding of mental illness.
Strategies to Combat Stigma
Various initiatives and strategies are crucial in reducing stigma and promoting understanding.
- Public awareness campaigns: Large-scale campaigns can educate the public about mental illness, challenge misconceptions, and promote help-seeking.
- Educational programs: Integrating mental health education into schools and workplaces can help normalize mental health concerns and reduce stigma.
- Personal storytelling: Sharing personal experiences can humanize mental illness and foster empathy and understanding.
Successful anti-stigma campaigns often combine multiple approaches, leveraging the power of personal narratives, educational materials, and widespread public outreach.
Improving the Quality and Availability of Mental Health Treatment
Improving the quality and expanding the availability of mental health treatment are paramount to addressing the crisis.
Expanding Access to Evidence-Based Therapies
Providing access to a wide range of evidence-based therapies is vital for effective treatment.
- Training more mental health professionals: Increasing the number of trained professionals, particularly in underserved areas, is critical.
- Increasing telehealth options: Utilizing telehealth expands access to care, especially for individuals in remote areas or with mobility challenges.
- Developing community-based programs: Community-based programs can provide accessible and affordable mental health services.
Examples of successful treatment models include Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and medication management, tailored to individual needs.
Investing in Mental Health Research
Continued investment in research is crucial for advancing our understanding, diagnosis, and treatment of mental illness.
- Funding for clinical trials: Investing in clinical trials is essential for testing the efficacy of new treatments and improving existing ones.
- Epidemiological studies: Understanding the prevalence and risk factors of mental illness helps inform public health initiatives and targeted interventions.
- Basic science research: Investing in basic science research helps unravel the biological mechanisms underlying mental illness, paving the way for more effective treatments.
Research helps to develop innovative treatments, improve diagnostic tools, and ultimately, enhance patient outcomes.
Promoting Integration of Mental and Physical Healthcare
Integrating mental and physical healthcare is vital for addressing the interconnectedness of these health domains.
- Collaborative care models: Collaborative care models bring together primary care physicians and mental health professionals to provide comprehensive care.
- Shared decision-making: Involving patients in treatment decisions empowers them and ensures care aligns with their preferences and needs.
- Improved communication between providers: Enhanced communication ensures seamless coordination of care and avoids potential conflicts or gaps in treatment.
Successful integrated care programs demonstrate improved patient outcomes, reduced hospitalizations, and increased patient satisfaction.
Conclusion
The challenges facing mental healthcare are multifaceted, encompassing limited access, high costs, pervasive stigma, and the need for improved treatment quality. These barriers significantly hinder individuals from seeking and receiving the care they need, resulting in significant personal suffering and a considerable societal cost. The urgent need for better mental health care cannot be overstated. Its impact reaches far beyond individual well-being, affecting families, communities, and the economy as a whole. We must advocate for improved mental healthcare policies, increased funding for research and treatment, and the dismantling of the stigma that prevents so many from seeking help. Let's work together to demand and create a system that provides truly better mental health care for everyone. For resources and support, please visit [Link to relevant organization 1] and [Link to relevant organization 2].

Featured Posts
-
 Souness On Rashford Aston Villas Transfer Pursuit Analyzed
May 03, 2025
Souness On Rashford Aston Villas Transfer Pursuit Analyzed
May 03, 2025 -
 Huntington Whiteleys Breathtaking White Lingerie A Style Icons Choice
May 03, 2025
Huntington Whiteleys Breathtaking White Lingerie A Style Icons Choice
May 03, 2025 -
 Souness Highlights Arsenals Champions League Threat A Team Above The Rest
May 03, 2025
Souness Highlights Arsenals Champions League Threat A Team Above The Rest
May 03, 2025 -
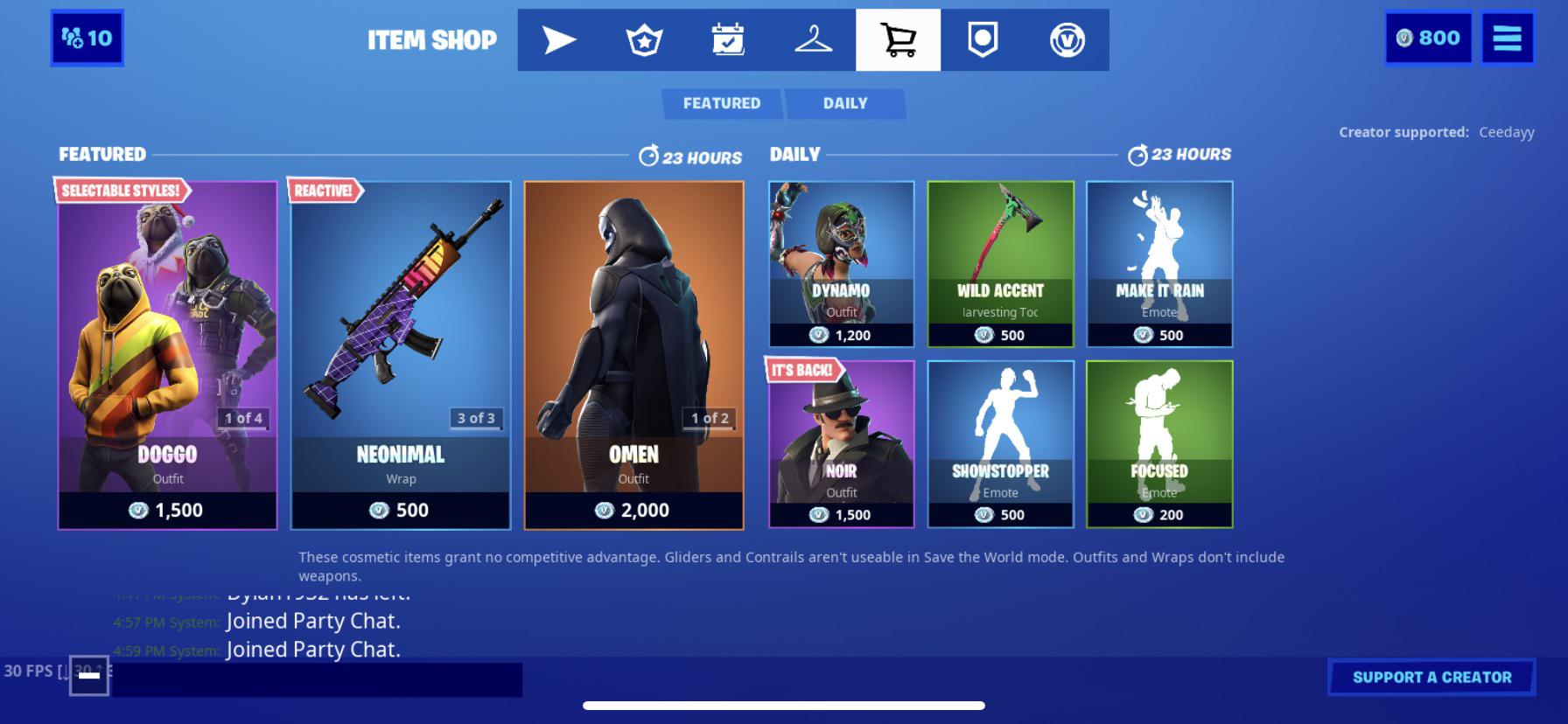 Latest Fortnite Item Shop Update Receives Backlash
May 03, 2025
Latest Fortnite Item Shop Update Receives Backlash
May 03, 2025 -
 Freedom Flotilla Drone Attack Near Maltese Waters
May 03, 2025
Freedom Flotilla Drone Attack Near Maltese Waters
May 03, 2025
