The Persistence Of Measles: Understanding Continued Transmission

Table of Contents
Factors Contributing to Measles Persistence
Several interconnected factors contribute to the ongoing transmission of measles. Understanding these complexities is crucial for developing effective control strategies.
Vaccine Hesitancy and Refusal
The rise of vaccine hesitancy and outright refusal is a major driver of measles persistence. Misinformation and anti-vaccine movements actively spread distrust in vaccines through various channels, significantly impacting vaccination rates. Social media and online platforms have amplified these narratives, often disseminating false claims about vaccine safety and efficacy.
- Common misconceptions: These include claims that the measles vaccine causes autism (debunked by numerous scientific studies), that natural immunity is superior to vaccine-induced immunity, and that vaccines are unnecessary in developed countries.
- Consequences of low vaccination rates: Reduced herd immunity leaves communities vulnerable to outbreaks, even affecting those who cannot be vaccinated due to medical reasons.
- Evidence-based decision-making: Reliable information from credible sources like the WHO, CDC, and national public health agencies is critical in countering misinformation and promoting informed vaccine choices. Examples of vaccine hesitancy-driven outbreaks include localized surges in measles cases within communities with low vaccination rates.
Gaps in Vaccination Coverage
Achieving high vaccination coverage is essential for establishing herd immunity, protecting populations from measles outbreaks. However, significant gaps remain globally, particularly in underserved and remote communities. Conflict, poverty, and displacement exacerbate these challenges, limiting access to vaccination services.
- Global vaccination coverage statistics: While global coverage has improved, many regions still fall short of the 95% target recommended by WHO for measles elimination.
- Factors affecting access to vaccines: These include limited healthcare infrastructure, lack of trained healthcare workers, logistical challenges in vaccine distribution, and socio-cultural barriers to vaccination.
- Strategies for improving vaccination coverage: This involves targeted outreach programs, mobile vaccination clinics, community engagement, and addressing the root causes of inequitable access.
Measles Virus Characteristics
The measles virus itself is highly contagious, making it particularly challenging to control. Its airborne transmission and ability to survive for several hours in the environment contribute to its rapid spread. The virus's incubation period (7-18 days) and the contagiousness before symptoms appear enable widespread transmission before cases are even identified.
- R0 value of measles: The measles virus has a high basic reproduction number (R0), meaning each infected individual can transmit the virus to many others.
- Modes of transmission: Primarily airborne through coughing and sneezing, it can also be transmitted through direct contact with respiratory secretions.
- Symptoms and contagious period: Measles symptoms include fever, cough, runny nose, rash, and conjunctivitis, and individuals are contagious from several days before the rash appears until several days after.
Understanding Measles Outbreaks
Rapid and effective response to measles outbreaks is crucial for minimizing their impact. This requires swift action, robust public health infrastructure, and community cooperation.
Outbreak Investigation and Response
Identifying and containing measles outbreaks involves a multi-step process. Public health agencies play a central role, utilizing surveillance systems, laboratory diagnostics, contact tracing, and quarantine measures.
- Steps involved in outbreak investigation: This includes case confirmation, epidemiological investigation (identifying contacts and risk factors), and mapping the spread of infection.
- Public health interventions: These include vaccination campaigns for susceptible individuals, case isolation, contact tracing, and public awareness campaigns.
- Challenges in managing outbreaks: Rapid spread in densely populated areas, limited resources in some settings, and vaccine hesitancy can hamper outbreak control efforts.
Global Spread and International Travel
International travel significantly facilitates the spread of measles across borders. Unvaccinated individuals can easily introduce the virus into countries with lower vaccination rates, leading to outbreaks.
- Examples of outbreaks linked to international travel: Numerous examples illustrate how imported cases can trigger widespread transmission within a community.
- Impact of travel restrictions: While travel restrictions can be effective in certain situations, they are not a long-term solution and often pose challenges to international cooperation.
- International collaboration in measles control: Global health organizations like WHO play a vital role in monitoring measles globally, providing technical assistance, and coordinating international responses.
Strategies to Combat Measles Persistence
Eliminating measles requires a multifaceted approach encompassing improved vaccination programs, enhanced surveillance, and strengthened global collaboration.
Improving Vaccination Programs
Increasing vaccine uptake requires multifaceted strategies. These include public awareness campaigns to address vaccine hesitancy, training healthcare providers to effectively communicate with patients, and developing innovative approaches to vaccine delivery.
- Effective communication strategies: Tailored messaging to specific communities, addressing concerns and misconceptions, and utilizing trusted community leaders are crucial.
- Community engagement initiatives: Involving communities in vaccine campaigns, addressing cultural barriers, and making vaccines accessible are all essential.
- Overcoming barriers to vaccination access: This includes tackling logistical challenges, financial barriers, and improving healthcare infrastructure in underserved areas.
Strengthening Surveillance and Monitoring
Robust surveillance systems are essential for early detection of outbreaks. Rapid laboratory diagnosis and timely data sharing among public health agencies are critical for effective response.
- Types of surveillance systems: Passive surveillance relies on healthcare providers reporting cases, while active surveillance involves proactive case-finding.
- Importance of rapid laboratory diagnosis: Confirming measles cases quickly allows for rapid implementation of control measures.
- Data analysis and interpretation: Analyzing data helps identify trends, risk factors, and vulnerable populations, informing public health strategies.
Conclusion: The Ongoing Fight Against Measles Persistence
The persistence of measles is a complex issue stemming from vaccine hesitancy, gaps in vaccination coverage, and the virus's inherent contagiousness. High vaccination coverage, effective outbreak response, and strong surveillance systems are crucial for preventing future outbreaks. Continued research and innovation in measles prevention and control are needed to move closer to a world free from this preventable disease. Learn more about measles and the importance of vaccination. Protect yourself and your community by ensuring timely vaccination and staying informed about measles outbreaks. Let’s work together to combat measles transmission and create a healthier future.

Featured Posts
-
 Preduprezhdenie Mada O Shtorme V Izraile Ekstrennye Mery Bezopasnosti
May 30, 2025
Preduprezhdenie Mada O Shtorme V Izraile Ekstrennye Mery Bezopasnosti
May 30, 2025 -
 Qst Alastqlal Ndal Wtdhyat Mn Ajl Alhryt
May 30, 2025
Qst Alastqlal Ndal Wtdhyat Mn Ajl Alhryt
May 30, 2025 -
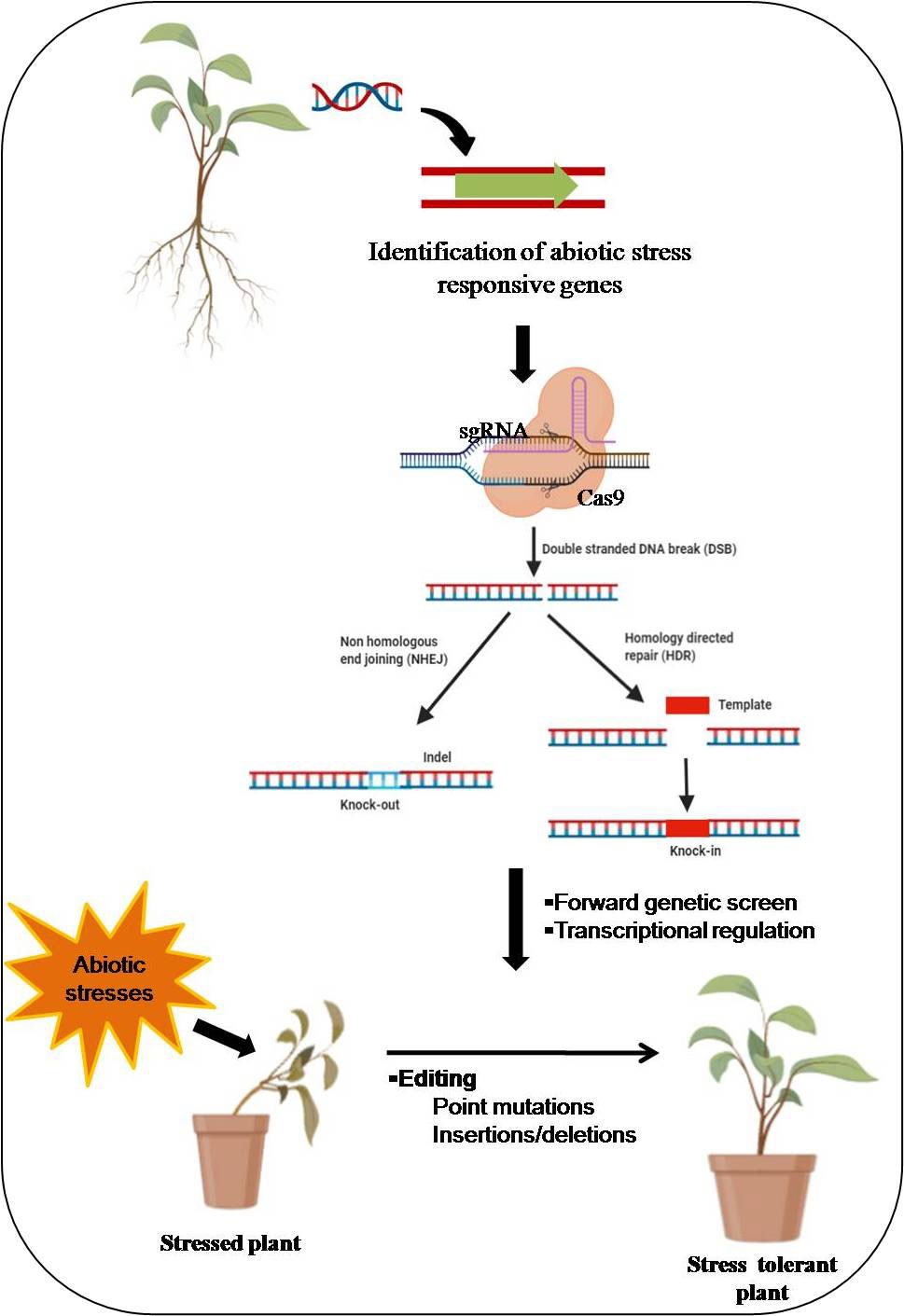 Crispr Gene Editing A Powerful System For Whole Gene Integration
May 30, 2025
Crispr Gene Editing A Powerful System For Whole Gene Integration
May 30, 2025 -
 Marine Le Pen Et Les Elections 2027 Un Possible Empechement Selon Jacobelli
May 30, 2025
Marine Le Pen Et Les Elections 2027 Un Possible Empechement Selon Jacobelli
May 30, 2025 -
 Han Taler Udenom En Dybdegaende Kig Pa Kare Quists Vaerk Gennem Ditte Okmans Udstilling
May 30, 2025
Han Taler Udenom En Dybdegaende Kig Pa Kare Quists Vaerk Gennem Ditte Okmans Udstilling
May 30, 2025
