The Emergence Of COVID-19 Variants BA.1 And LF.7 In India: A Public Health Perspective
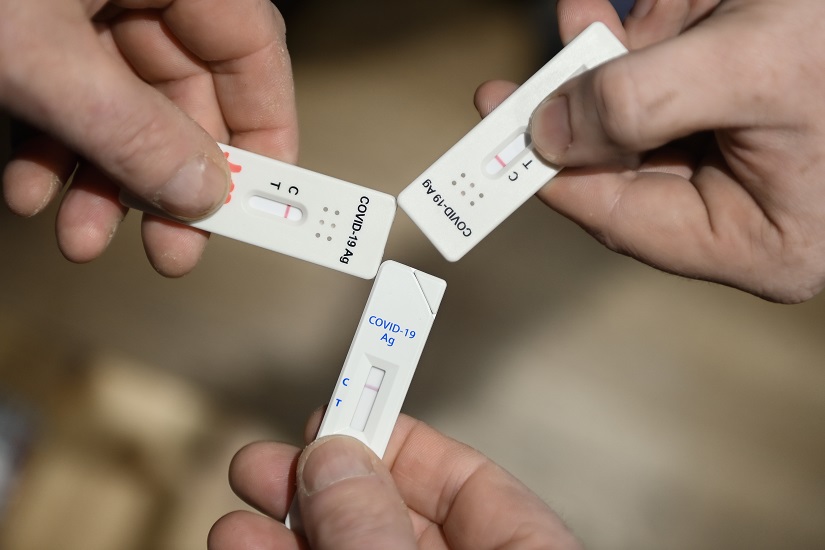
Table of Contents
Characteristics and Transmission of BA.1 in India
Genetic Makeup and Mutations
BA.1, a subvariant of Omicron, carries a distinct set of mutations compared to the original Omicron variant and earlier strains. These mutations affect various aspects of the virus's behavior, including its transmissibility and ability to evade the immune response.
- Spike Protein Mutations: BA.1 possesses key mutations in the spike protein (e.g., B.1.1.529.1, K417N, G446S, Q493R, G496S, Q498R, N501Y, Y505H), impacting its ability to bind to human cells and potentially affecting vaccine efficacy. (Specific scientific sources citing these mutations and their effects would be inserted here.)
- Prevalence: Data on the geographic distribution of BA.1 in India (which would be sourced from credible epidemiological studies) needs to be included here, showing its prevalence in various states and regions. Maps or charts visualizing this data would greatly enhance the article's impact.
Transmission Dynamics
The transmission dynamics of BA.1 in India exhibited rapid community spread, exceeding the transmissibility of previous variants in many regions. (Insert R0 values if available and sourced from reliable studies). The ease with which BA.1 spread underscores the need for proactive public health measures.
- Community Spread: BA.1 demonstrated a significant capacity for community transmission, surpassing earlier COVID-19 variants in its speed of spread. (Cite sources demonstrating community spread)
- Vulnerable Populations: Particular attention should be paid to the impact of BA.1 on vulnerable populations, such as the elderly, individuals with comorbidities, and those in densely populated areas. (Include data on hospitalization and mortality rates in these populations, sourced from relevant studies)
Clinical Manifestations
While generally less severe than some earlier variants like Delta, BA.1 still caused a range of clinical manifestations. Many cases were asymptomatic or presented with mild symptoms. However, severe cases requiring hospitalization were still reported, particularly among vulnerable groups.
- Symptom Comparison: A comparison of BA.1 symptoms with those of previous variants (Delta, Alpha) would provide valuable context. (Include information on common symptoms: fever, cough, fatigue, loss of taste/smell, etc., citing relevant studies.)
- Severity and Hospitalization Rates: Include data on hospitalization rates and the severity of BA.1 infections in India, comparing them to previous variants. (Include data from credible sources like the Indian Council of Medical Research (ICMR) or the Ministry of Health and Family Welfare.)
Characteristics and Transmission of LF.7 in India
Genetic Makeup and Mutations
LF.7, another Omicron sub-variant, displays its own unique set of mutations. (Detailed information on the specific mutations and their impact would be included here, with citations from peer-reviewed research). Comparison with BA.1’s mutations would highlight similarities and differences, offering insights into their relative transmissibility and potential immune evasion capabilities.
- Key Mutations of LF.7: List the key mutations found in LF.7 and their potential impact on transmissibility, virulence, and immune escape. (Cite scientific publications detailing the genetic characteristics of LF.7.)
- Comparison with BA.1: A comparative analysis of the mutations in LF.7 and BA.1 would provide a better understanding of their differences in infectivity and pathogenicity.
Transmission Dynamics
Analysis of LF.7's spread in India requires a detailed examination of its transmission patterns, R0 value (if available), and comparison to BA.1's spread. (Insert relevant data and charts visualizing transmission dynamics, comparing BA.1 and LF.7 spread. Source data from credible epidemiological studies). This analysis will highlight any potential differences in transmissibility and ability to evade immunity.
- Immune Evasion: Discuss any evidence suggesting LF.7 might be more adept at evading the immune response compared to BA.1 or other variants. (Cite relevant studies exploring immune evasion mechanisms.)
- Geographic Distribution: Present data on the geographic distribution of LF.7 in India, comparing it to that of BA.1. Highlight any regions where LF.7 was particularly prevalent.
Clinical Manifestations
The clinical presentation of LF.7 infections needs to be analyzed, comparing it to BA.1 and other variants. (Include data on symptom severity, hospitalization rates, and mortality rates associated with LF.7 infections, appropriately sourced).
- Severity and Outcomes: Compare the severity of LF.7 infections with those caused by BA.1 and other variants. (Cite peer-reviewed research or reports from official health organizations.)*
- Comparison with BA.1: Highlight any significant differences in clinical manifestations between LF.7 and BA.1 infections.
Public Health Response and Preparedness
Vaccination Strategies
The efficacy of existing COVID-19 vaccines against BA.1 and LF.7 needs to be assessed. (Data on vaccine effectiveness against these variants, sourced from clinical trials and real-world studies, needs to be presented). The Indian vaccination rollout and its impact on the spread of these variants must also be discussed.
- Booster Campaigns: Discuss the role of booster shots in enhancing protection against BA.1 and LF.7 and their effectiveness in India.
- Vaccine Accessibility: Analyze the accessibility of vaccines across different regions of India and identify any disparities.
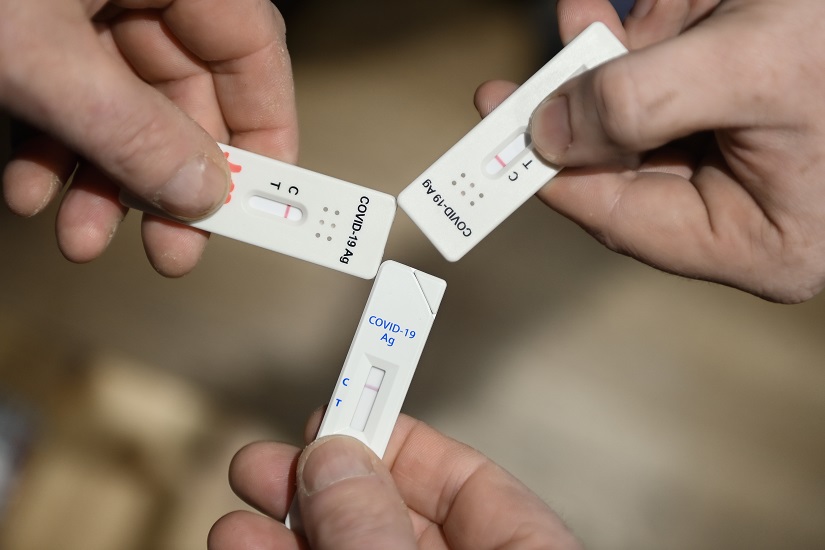
Surveillance and Testing
Genomic surveillance plays a crucial role in detecting and tracking the emergence and spread of new variants like BA.1 and LF.7. (Discuss the capacity of India’s genomic surveillance system and the importance of timely detection). The effectiveness of testing and contact tracing measures in containing the spread of these variants also needs detailed assessment.
- Genomic Sequencing: Describe India's capacity for genomic sequencing and its role in identifying new variants. (Include data on the number of samples sequenced and the timeliness of sequencing results.)
- Testing Capacity: Discuss the testing capacity in India and its effectiveness in detecting and managing cases of BA.1 and LF.7 infections.
Non-Pharmaceutical Interventions
The effectiveness of non-pharmaceutical interventions (NPIs) such as mask mandates, social distancing, and hygiene protocols in controlling the spread of these variants needs careful consideration. (Assess the impact of NPIs in reducing transmission, citing data and studies on their effectiveness).
Conclusion
The emergence of COVID-19 Variants BA.1 and LF.7 in India highlighted the ongoing challenges in managing the pandemic. While generally less severe than earlier variants, their high transmissibility necessitates continued vigilance. Effective vaccination strategies, robust genomic surveillance, and the appropriate implementation of non-pharmaceutical interventions are crucial for mitigating the impact of these and future variants. Continued genomic surveillance, effective vaccination strategies, and robust public health measures remain crucial in managing the ongoing threat of emerging COVID-19 variants BA.1 and LF.7 in India and protecting the population. Proactive preparedness and a flexible approach to public health strategies are vital for safeguarding India's future against emerging COVID-19 threats.
Featured Posts
-
 Giro D Italia Live Stream Watch Mens Cycling Online
May 31, 2025
Giro D Italia Live Stream Watch Mens Cycling Online
May 31, 2025 -
 Finding Your Good Life Practical Steps For Personal Transformation
May 31, 2025
Finding Your Good Life Practical Steps For Personal Transformation
May 31, 2025 -
 Reversing Brexit Harm Boes Bailey Advocates For Deeper Eu Trade
May 31, 2025
Reversing Brexit Harm Boes Bailey Advocates For Deeper Eu Trade
May 31, 2025 -
 Auction Preview Banksys Broken Heart Wall Art
May 31, 2025
Auction Preview Banksys Broken Heart Wall Art
May 31, 2025 -
 Dragon Den Star Invests In Chafford Hundred Padel Courts
May 31, 2025
Dragon Den Star Invests In Chafford Hundred Padel Courts
May 31, 2025
