Improving Mental Health Care: A Critical Look At Current Systems
Table of Contents
Accessibility Challenges in Mental Healthcare
Access to mental healthcare remains a significant hurdle for many, hindered by a complex interplay of geographic, financial, and systemic barriers.
Geographic Barriers
The unequal distribution of mental health professionals creates significant disparities in access to care. Rural communities and underserved populations are disproportionately affected by a shortage of psychiatrists, psychologists, and other mental health specialists.
- Lack of Transportation: Limited public transportation options and long distances to the nearest mental health clinic make it incredibly difficult for individuals in rural areas to access care.
- Long Waiting Lists: Even in areas with available services, long waiting lists for appointments can delay crucial treatment, exacerbating existing conditions.
- Limited Telehealth Options: While telehealth offers a promising solution, its reach in rural areas is often limited by unreliable internet access and a lack of digital literacy.
Statistics reveal stark disparities: rural areas often have only one mental health professional for every 10,000 residents, compared to urban areas with a much higher ratio. This geographical imbalance urgently needs addressing through strategic investments in rural healthcare infrastructure and the expansion of telehealth services.
Financial Barriers
The high cost of mental healthcare is another major obstacle. Therapy sessions, medication, and hospitalization can be prohibitively expensive, placing a significant financial burden on individuals and families.
- High Insurance Premiums, Deductibles, and Co-pays: Many insurance plans have high out-of-pocket costs, making mental healthcare unaffordable for many individuals.
- Lack of Affordable Options for Uninsured or Underinsured Individuals: Millions lack adequate health insurance, leaving them with limited or no access to affordable mental health services.
- Cost of Prescription Medication: The price of psychiatric medications can be substantial, further hindering access to treatment for those with limited financial resources.
Increased government funding for mental health services and comprehensive insurance reforms, including parity laws that ensure equal coverage for mental and physical healthcare, are crucial steps towards addressing these financial barriers.
Systemic Barriers
Navigating the mental healthcare system itself can be a daunting task, further hindering access to care.
- Complex Referral Processes: The process of obtaining a referral to a specialist often involves numerous steps and delays, potentially delaying treatment.
- Difficulty Finding In-Network Providers: Many insurance plans have limited networks of mental health providers, forcing individuals to choose between higher out-of-pocket costs or limited access.
- Lack of Clear Information about Available Services: The lack of readily available and user-friendly information regarding mental health services creates confusion and frustration for individuals seeking help.
Streamlining referral processes, expanding provider networks, and implementing comprehensive patient navigation programs can significantly improve the accessibility of mental healthcare.
Quality and Effectiveness of Mental Health Services
Beyond access, the quality and effectiveness of mental health services are equally critical for improving mental health outcomes.
Treatment Gaps
Current mental health treatments often fall short of providing truly personalized and effective care.
- Insufficient Use of Evidence-Based Practices: Many clinicians are not utilizing evidence-based treatments, leading to suboptimal outcomes for patients.
- Lack of Culturally Competent Care: Mental healthcare should be tailored to the individual’s cultural background and beliefs to maximize effectiveness.
- Limited Access to Specialized Treatments: Access to specialized treatments, such as intensive therapy or medication management, is often limited.
Integrating innovative treatments, implementing personalized medicine approaches, and fostering culturally competent care are vital for improving treatment efficacy.
Stigma and Discrimination
The pervasive stigma surrounding mental illness discourages many from seeking help.
- Social Stigma: Negative attitudes and misconceptions about mental illness prevent individuals from openly discussing their struggles and seeking support.
- Discrimination in Employment and Housing: Individuals with mental health conditions often face discrimination in employment and housing, further isolating them and worsening their prognosis.
- Fear of Judgment: The fear of judgment from family, friends, and colleagues prevents many from seeking professional help.
Public awareness campaigns, educational initiatives, and community-based support groups can help reduce the stigma and encourage help-seeking behavior.
Integration of Physical and Mental Healthcare
Integrating physical and mental healthcare is crucial for holistic well-being.
- Benefits of Collaborative Care Models: Collaborative care models, where mental and physical health professionals work together, improve patient outcomes.
- Improved Patient Outcomes: Integrated care approaches lead to improved treatment adherence and better overall health outcomes.
- Cost-Effectiveness: By addressing both physical and mental health concerns simultaneously, integrated care can ultimately prove more cost-effective.
Successful examples of integrated care programs demonstrate the benefits of this approach and should be scaled up for broader implementation.
Potential Solutions for Improving Mental Healthcare
Addressing the systemic challenges in mental healthcare requires a multi-pronged approach.
Increased Funding and Investment
Increased government investment is crucial to support research, workforce development, and community-based services.
- Funding for Mental Health Research: Investment in research is needed to develop more effective treatments and interventions.
- Training Programs for Mental Health Professionals: More training programs are needed to increase the number of mental health professionals and enhance their skills.
- Expansion of Community Mental Health Centers: Expanding community mental health centers increases access to affordable care for underserved populations.
Policy and Legislative Changes
Policy reforms are essential to expand access and improve the quality of care.
- Expanding Medicaid Coverage for Mental Health Services: Expanding Medicaid coverage ensures that more low-income individuals can access mental healthcare.
- Mandating Mental Health Benefits in Employer-Sponsored Insurance Plans: Requiring mental health benefits in employer-sponsored plans ensures better coverage for many employees.
- Stronger Regulations for Mental Health Facilities: Stronger regulations ensure higher standards of care in mental health facilities.
Technology and Innovation
Technology can play a significant role in enhancing access to mental healthcare.
- Telehealth Expansion: Expanding telehealth services makes mental healthcare more accessible to individuals in remote areas and those with mobility limitations.
- Development of Mobile Apps for Mental Health Support: Mobile apps provide convenient access to self-help resources, information, and support.
- Utilization of AI in Mental Health Diagnosis and Treatment: AI-powered tools can assist in diagnosis, treatment planning, and monitoring of patients.
The Path Forward in Improving Mental Health Care
Improving mental health care requires a concerted effort to address accessibility, quality, and affordability challenges. This necessitates increased funding, policy changes, technological advancements, and a significant reduction in stigma. By implementing the solutions outlined above, we can create a more equitable and effective mental healthcare system. We must advocate for better mental health services and actively work towards improving mental health outcomes for everyone. Let's make improving mental health care access a shared priority, ensuring that individuals struggling with mental health issues receive the timely and effective care they deserve. Start advocating for better mental health services in your community today.
Featured Posts
-
 Arc Raiders Second Public Test What To Expect
May 02, 2025
Arc Raiders Second Public Test What To Expect
May 02, 2025 -
 Kshmyr Pakstany Army Chyf Ka Skht Mwqf
May 02, 2025
Kshmyr Pakstany Army Chyf Ka Skht Mwqf
May 02, 2025 -
 Enexis Blokkeert Duurzame School Kampen Dagvaardt Energieleverancier
May 02, 2025
Enexis Blokkeert Duurzame School Kampen Dagvaardt Energieleverancier
May 02, 2025 -
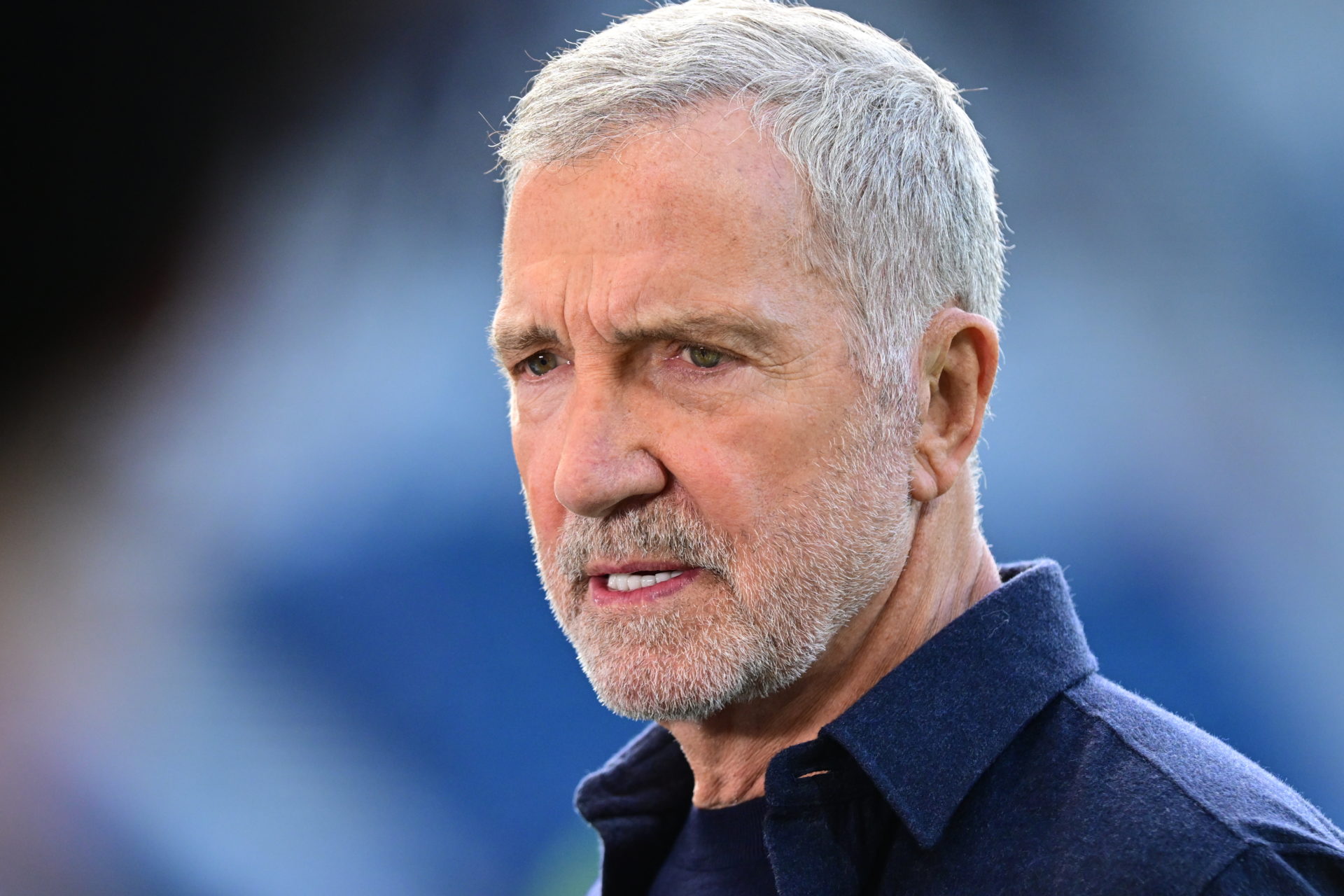 Graeme Souness Reveals His Premier League Favourite Player
May 02, 2025
Graeme Souness Reveals His Premier League Favourite Player
May 02, 2025 -
 Ex Mp Rupert Lowe And Reform Shares Report Details Unlawful Harassment Allegations
May 02, 2025
Ex Mp Rupert Lowe And Reform Shares Report Details Unlawful Harassment Allegations
May 02, 2025
